You often hear the word “growth” in health and social care. But can we really define growth in health and social care?
Many people think growth means bigger buildings or budgets. Real growth is deeper; it means improving every day. It makes care safer, more effective, and focused on the person. Growth is a commitment to higher standards, benefiting staff, services, and, most importantly, the people we support.
In this article, we will define growth in health and social care and examine it in three ways: personal growth, service growth, and outcome growth. We will also investigate how to measure growth, what helps it, and what blocks it. By the end, you will understand how daily growth makes a big difference.
What Does Growth Meaning Health and Social Care?

Many think growth is about numbers, such as more staff or bigger budgets. But what is growth in health and social care? The real growth is about doing better. It is about improving skills, quality, and capacity.
Growth is not about being bigger. It is about improving every day. For example, imagine a care home that wants to improve dementia support. Staff attend training to learn new methods, gaining knowledge and confidence. Residents benefit from activities that will enhance mood and memory. This shows real growth. Staff skills grow. Service quality improves. Residents achieve better outcomes.
Growth happens in many ways. A support worker might learn new safety rules. A care team might improve communication to reduce mistakes. A service might adopt new technology to track patient progress. The goal is the same: helping staff and teams reach higher standards. Growth ensures people get better support and independence.
In practice, growth is easy to see. People get better care, staff feel confident and valued, and services run more smoothly. Every small improvement has a big, lasting impact.
Why Do We Talk About Growth in Health and Social Care?
Health and social care are always changing. Our population is getting older, mental health needs are rising, and technology keeps changing how care is delivered.
Growth keeps services safe, effective, and person-centred. Without it, care can become outdated or unsafe. For example, consider a community mental health team. If they do not learn new therapy methods, their care might not meet patients’ needs. They might also miss important changes if they do not use digital tools to track patients.
Growth helps staff learn new techniques, and it also brings new technology into care. As a result, services stay flexible and responsive. Growth also promotes fairness. It ensures everyone gets proper support. Staff feel confident and capable. Morale improves, burnout decreases.
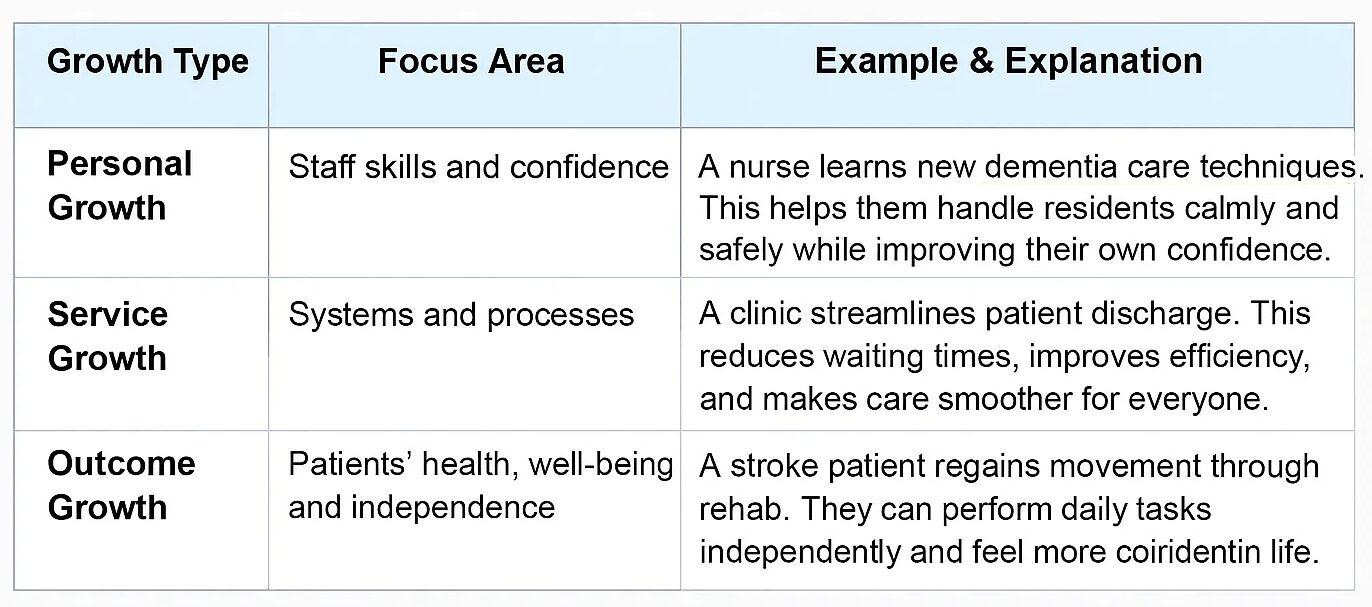
Define Growth in Health and Social Care Through Three Key Areas
Growth happens in three main ways, and together, they improve care for everyone. For example, personal growth helps staff learn new skills. Service growth makes systems work better. Thus, outcome growth helps patients stay healthy and happy. By tracking progress, care keeps getting better each day.
Here’s an illustration of how each form of growth functions in practice:
How to Measure Growth in Health and Social Care?

Measuring growth helps us see whether care is truly improving. It clearly shows what’s working well and what still needs attention. We often use Key Performance Indicators (KPIs) to track this progress in health and social care. These are simple measures that show if changes are making a real difference.
Here are some key ways to measure growth:
- Patient outcomes: This means checking if people are getting healthier and feeling better. Care improves when patients recover faster, have fewer hospital readmissions, or report less pain and stress. For example, if a care team helps an older patient walk again after surgery, that shows strong patient outcomes.
- Quality ratings: Quality ratings come from organisations like the CQC in the UK. They show how good care really is. Inspections focus on safety, leadership, effectiveness, and how staff treat people. For example, if a care home rises from “Requires Improvement” to “Good”, it indicates that the service has expanded and improved.
- Readmissions and escalations: Fewer emergencies and hospital readmissions mean care is working well. It shows that people are being supported properly the first time, so they don’t need to come back with the same problem. For instance, when a diabetic patient manages their condition with regular check-ins, it helps them stay stable. As a result, it also reduces emergency visits.
- Staff performance: Growth is not just about patients; it’s also about staff. Besides, when staff feel confident, it creates a supportive environment. This kind of growth improves morale and makes staff proud of their work.
- Access and outreach: Growth also means reaching more people, especially those struggling to get care. For example, a new outreach programme might bring health checks to rural villages or home visits to older adults. When more people get help, services become fairer and more inclusive.
All these indicators work together to show how much progress is being made. Some measures look at outcomes, showing what happens to people. Others track processes, showing how care is delivered. Meanwhile, structural measures focus on the systems and resources in place. We use outcome, process, and structure measures. Also, balancing measures check for unintended consequences. Tools like audits and feedback help check growth. Knowing how to measure health and social care growth makes progress clear and meaningful.
What Helps Growth Happen in Health and Social Care Settings?
Growth does not happen by accident. It needs the right support, teamwork, and learning. Employees who feel valued and given the appropriate tools provide better care.
Here are a few crucial factors that help growth happen:
CPD in Health and Social Care
One of the most popular ways of development is Continuous Professional Development (CPD). This keeps them updated with the latest care methods. For example, a nurse trained in dementia care can give safer, better support. Also, training builds confidence and pride, leading to happier teams and better care. For example, a nurse who learns new dementia care techniques can give safer and more effective support. Such training also makes staff feel confident and proud of their work. Over time, this leads to better care and happier teams.
Supportive Leadership in Care
Good leaders play a big role in growth. They guide their teams, listen to their ideas, and help solve problems calmly. As a result, staff get support from their leaders, feel calm, and are more eager to improve. For example, a manager who praises effort and gives helpful feedback builds a positive, caring team. Strong leadership also keeps staff working together with clear goals.
Digital Transformation in Healthcare
Technology makes care faster, safer, and easier. For example, electronic records help doctors and carers share information quickly. This reduces mistakes. Also, AI can organise data and remind staff about important updates. With these tools, workers can spend more time caring for people.
Multi-Agency Collaboration
We’re all aware that teamwork leads to greater achievement. In fact, health care, social services, and charity contribute valuable ideas and resources. Together, they can address issues that no one can resolve alone. When everyone communicates and takes responsibility, care becomes more complete, nurturing, and efficient.
In short, growth happens when people learn, lead, use technology wisely, and work as one team. With this support, staff and patients can grow and succeed together.
What Prevents Growth in Health and Social Care?
Sometimes, growth slows down because of a few common barriers. Each one can make it harder for services and staff to move forward.
Limited Funding
Limited funding, for instance, makes it hard for services to grow because they cannot buy new tools or provide proper training. Without enough resources, even small improvements become difficult.
Employee shortages and dissatisfaction
Staff shortages also create big problems. Overworked people feel tired and stressed, which makes it harder to stay focused and find time for improvement.
Outdated Systems
Traditionally, old systems can also slow progress because teams often keep using old methods and resist change. As a result, they become unsure about new ways of working, and progress starts declining.
Lack of Training or Leadership
A lack of training or strong leadership can also stop growth. Because when staff don’t feel guided or supported, they lose motivation and confidence to improve.
Solutions include mentorship, small improvement cycles (like PDSA), reducing workload, and mindfulness training. Even small changes can remove barriers.

Let’s know what PDSA is:
PDSA stands for Plan-Do-Study-Act. It is a simple, practical method for testing and improving processes. Here’s a breakdown:
- Plan – Decide what change you want to make and plan how to test it.
- Do – Try the change on a small scale.
- Study – Look at the results and see what worked and what didn’t.
- Act – If it worked, implement it more widely. If not, adjust and try again.
PDSA helps health and social care teams make improvements safely, step by step, without risking big problems.
Why Growth Matters for Patients and Staff
Continuous improvement in healthcare means always finding ways to make care safer, faster, and better. Also, a growth mindset helps them learn, fix mistakes, and help patients more safely. The benefits of growth in health and social care are as follows:
- Patients: They feel safe, supported, and more independent. They also get better care.
- Staff: They feel skilled, valued, and confident. As a result, burnout goes down.
- Services: They run more smoothly, stay fair, and respond faster to people’s needs.
Actually, growth creates a positive vibe. When services improve, patients thrive. Thriving patients motivate staff. The benefits ripple across the system every day.
Final Thoughts: Keep Growing to Keep Caring
Coming to the end, growth is an attitude that builds staff, services, and better care. When we focus on continuous improvement, we can truly define growth in health and social care.
Every small step counts. So reflect, learn, and test adjustments. Use the PDSA cycle for small changes. Even tiny improvements make a big difference over time.
Interested in a health and social care course? Check out the Health and Care courses at the School of Health Care site.
FAQs
1. What is the definition of growth in health?
Growth in health means improving skills, care quality, and outcomes for patients and staff.
2. What is development in health and social care?
Development is learning, improving knowledge, and gaining new abilities to provide better care.
3. What is the basic definition of growth?
Growth is getting better, improving, or increasing in skill, size, or quality.
4. What are the principles of growth in health and social care?
Key principles include safety, effectiveness, person-centred care, and continuous improvement.
5. What is meant by the term growth in health and social care?
It means improving staff skills, service quality, and outcomes for the people receiving care.
6. What is growth in short answer?
Growth is progress or improvement over time.
7. What best describes growth?
Growth is becoming better, learning, and improving results or performance.
8. What is health growth?
Health growth is improving people’s physical, mental, and social well-being.
9. What is growth and development in healthcare?
It is improving skills, knowledge, and care systems to support better patient outcomes.
10. What are the 4 principles of growth?
The four principles are safety, effectiveness, person-centred care, and continuous improvement.